 |
| From http://stickmancommunications.co.uk/Keyring-Card-Fibromyalgia |
Serendipity strikes again! On Facebook, I saw https://www.facebook.com/PaleoDietNewZealand/posts/763653980371516 . That linked to Fibromyalgia and non‑celiac gluten sensitivity: a description with remission of fibromyalgia.
For people unfamiliar with scientific terms, here are some definitions:-
Non-celiac gluten sensitivity: A reaction to gluten, not due to Celiac (Coeliac in the U.K.) Disease.
Remission: (medicine) An abatement or lessening of the manifestations of a disease.
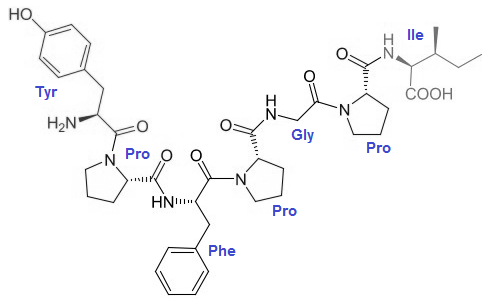
So, is Gliadorphin-7 (formed during the digestion of gluten) to blame?
 |
| Probably. |
Could Beta CasoMorphin-7 (formed during the digestion of A1 cow's milk) also be a problem?
 |
| Possibly. |
Is Increased/Excessive Intestinal Permeability allowing the above large molecules to pass through insufficiently tight junctions?
 |
| Definitely, maybe. |
Is there really no cure for Fibromyalgia? It's possible to tighten-up insufficiently tight junctions. Insufficiently tight junctions can be caused by:-
1. Insufficient sun exposure, causing hypovitaminosis D. See http://www.ncbi.nlm.nih.gov/pubmed/?term=%22Vitamin+D%22[All+Fields]+AND+%22tight%20junction%22+AND+hasabstract[text]
2. Excessive consumption of oils high in polyunsaturated fatty acids. See Dietary Fat Can Modulate Intestinal Tight Junction Integrity.
3. Excessive consumption of Wheat. See http://www.ncbi.nlm.nih.gov/pubmed/?term=%22Wheat%22[All%20Fields]%20AND%20%22tight%20junction%22[All%20Fields]%20AND%20hasabstract[text]%20AND%20%22humans%22[MeSH%20Terms]
4. Excessive exercise. See Shedding Some Light on the Leaky Gut <> Exercise Connection. Plus: 20+ Things You Should or Shouldn't Do to Protect and Restore the Integrity of Your Intestinal Wall.
5. Lack of dietary Sulphur. See Sulphation and Autism: What are the links? A good source of sulphate is Epsom Salts.
See also Physiology and Immunology of Digestion.
And finally...
If a science person ever tells you "Increased/Excessive Intestinal Permeability a.k.a. "Leaky gut" just doesn't exist because, you know, I'm a scientist.", point out that it's an Appeal from authority fallacy, and demand that they provide high quality evidence to support their statement.
Because, you know, I'm a retired Electronic Engineer! :-)




